NEWS RELEASE September 2019
The Future of Biopharmaceuticals will Depend on Perceived Value vs Cost
The National Institute for Health and Care Excellence (NICE) in the U.K has approved several CAR-T therapies even though the cost may be hundreds of thousands of dollars. The rationale is that the benefits will be long lasting and result in average costs per Quality Adjusted Life Year (QALY) gained which are within the guidelines.
NICE says it generally considers that interventions costing the National Health Service (NHS)
less than £20,000 per QALY gained are cost effective and those costing up to £30,000 per QALY gained might, with certain conditions satisfied, be considered cost effective.
The biopharmaceutical industry is making rapid progress to develop drugs to cure or mitigate diseases. However, this progress is coming with increased costs.
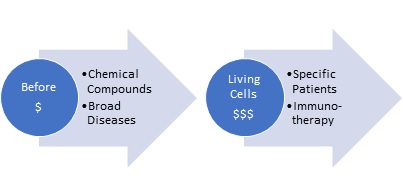
Costs increased as the healthcare industry expanded from using chemical compounds and treating broad diseases to utilizing living cells and creating drugs for specific individuals with CAR-T and other therapies. Even if there is no increase in the cost reimbursement per QALY, new medicines will increase the number of people who will benefit.
This results in a steadily increasing cost of healthcare as a percentage of GDP. This will require tougher decisions about how care is allocated. The optimum program should take into account
1 A more useful definition than QALY
2 The need to allocate health care expenditures as part of a broader program to maximize life quality
3 Integration of two additional metrics
a. Discounted future value
b. Tribal factor
A more useful definition than QALY
QALY is widely used around the world to determine the cost/benefits of treatment. One year of perfect health equals one QALY. One year of less than perfect health has a quality of life (QoL, or utility value) between 0–1. Death has a utility value of 0 (a respondent could choose to record a score below zero – worse than death – where, for instance, they are experiencing severe distress and/or possibly a terminal illness).
QoL has five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/ depression, each of which can be at one of three levels of severity, for example: no problems, some/moderate problems and extreme problems. A new five-level version can describe 243 unique combinations.
The problem with QALY is that the definition of perfect is far below the aspirations of anyone. A prisoner in solitary confinement could be higher on the list for a heart transplant than most individuals. The solider who falls on the grenade has elevated one minute of life quality above decades of life quantity. The average person would rather live to 80 and enjoy life than live to 100 without ever experiencing life’s more risky pleasures.
There is a metric which is better than QALY and will have common acceptance. It is Quality Enhanced Life Days (QELD). It simply quantifies the decisions people have made and are making to improve their life quality.
The need to allocate health care expenditures as part of a program to maximize life quality. With all the new therapies there is a real value in continuing to increase expenditures as a percentage of GDP. This decision can be best made by using QELD as a common metric to decide how expenditures are allocated. An example would be climate change vs healthcare. There is a world wide movement for a very expensive program to reduce CO2 emissions. What share of GDP should go to fight climate change versus medical treatment? QELD can be the metric to best make this decision.
Integration of Two Additional Metrics
QELD has to be determined based on the intrinsic value but with these additional metrics. One is the discounted future value. A medical treatment may have immediate benefits whereas investment in programs to decrease greenhouse gases may not have tangible benefits for many decades. The other metric is the tribal factor. Most people prioritize family life quality followed in descending order by friends and neighbors, city, and finally country. The lower concern for individuals in other countries is reflected in the foreign aid budgets of wealthy nations. It is typically far less than 1% of GDP.
McIlvaine has provided in depth analysis of the use of QELD, discounted future value, and the tribal factor in its consulting activities. Cardinal Health contracted with McIlvaine to help them determine whether they should be offering single use or reusable surgical gowns. Single use surgical gowns are discarded and replaced adding to the world’s CO2 burden. Washing and reusing gowns provides risks of waterborne disease.
The analysis concluded that the quantity of CO2 emitted from manufacturing 17 million gowns per year was miniscule as was the risk of water borne disease from reusables. The difference for hospital patients living near the hospital was that the washing risks would be immediate and would affect them whereas the greenhouse gas risks were long term and unlikely to affect them as much as it would those living near the equator.
More information on this study is shown at Sustainability Universal Rating System An article on the subject was featured in https://www.healthcaredevelopmentmagazine.com/article/quality-enhanced-life-days-a-new-metric-for-hospital-sustainability.html. For more information on this initiative contact Bob McIlvaine at This email address is being protected from spambots. You need JavaScript enabled to view it. cell 847 226 2391



